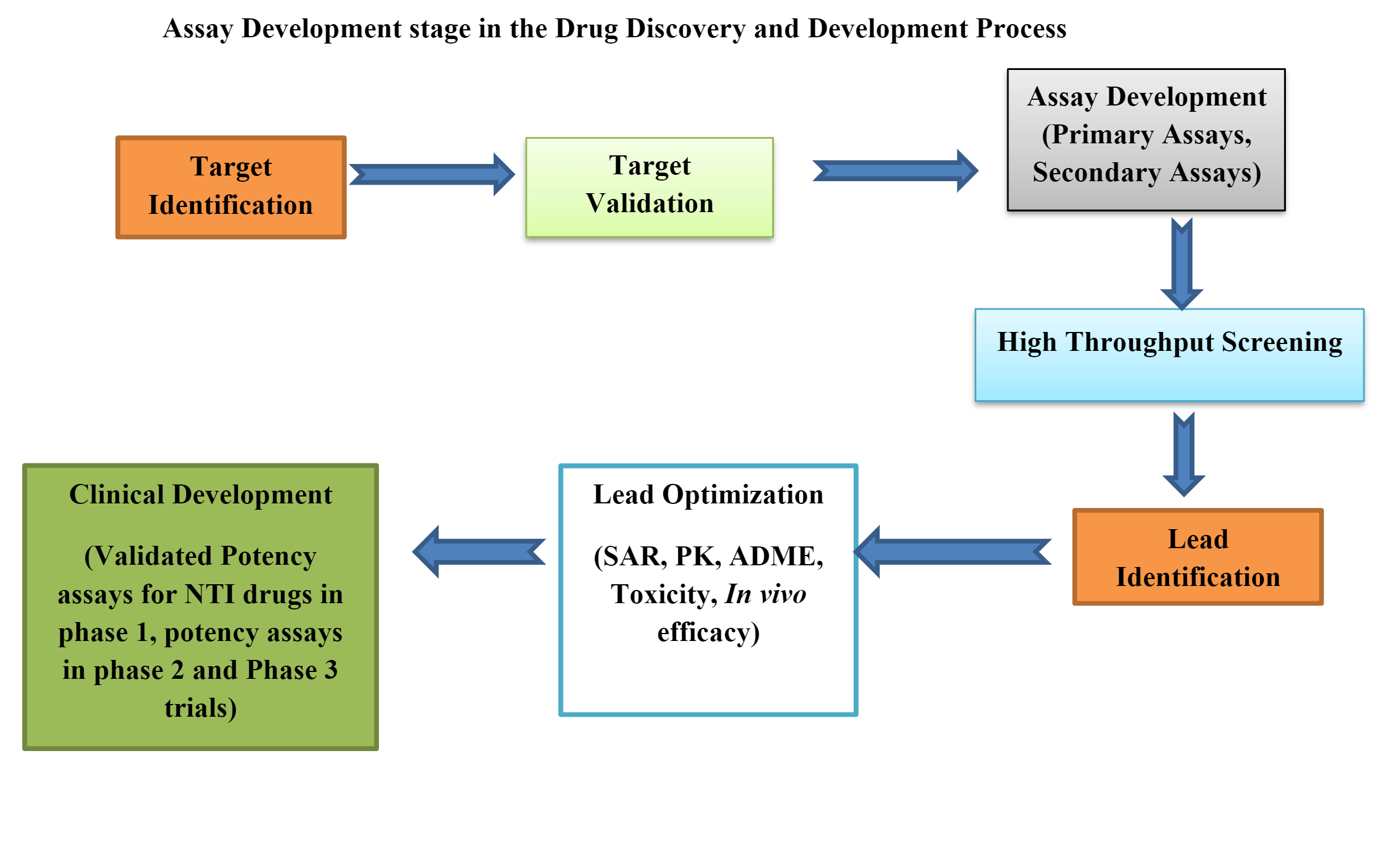
Bioassays are involved in each stage of drug discovery, starting from Target Identification until discovering the Lead compound. Bioassays provide valuable information which displays the therapeutic potency of a drug under investigation.
The data generated during bioassay also plays a vital role in drug development and quality control of finished biological products. Properly designed Bioassays help in assessing the biological effect, activity, signal transduction process, and receptor binding ability of drug product or biologic on a biological target (proteins) when compared to a reference or standard over a suitable biological system.
The pharmaceutical and biotech companies involved in drug discovery and development are continuously challenged with developing biologically relevant assays for the analysis of multiple potential mechanisms.
The process involves the use of quality critical reagents, use of specific cell lines, and purified test drug and reference drug products which at times may become a constraint. Most of these activities require sufficient time, which may become a limiting factor to biopharma manufacturers.
It is worth outsourcing activities to reputed CRO service providers to save time in developmental efforts and also to have an unbiased opinion on the functional activities of the drug product.
Veeda Group has qualified and experienced scientists to design, develop, execute, and validate the Bioassays for companies and provides premier bioassay services (in vitro and in vivo) that generate meaningful data to support pharmaceutical and biotech companies in their drug discovery and development journey.
Veeda Group’s Experience in Development and Execution of Bioassays include:
- Plaque Reduction Neutralization Test (PRNT assay)
- In Vitro Skin Sensitization Human Cell Line Activation test (h-CLAT assay)
- Nab Assay
- Assay Development (Pharmacodynamics, Pharmacokinetics, Immunogenicity, and Biomarker Assessment)
- In Vivo Bioassays for drug molecules like Luteinizing Hormone, Epoetin, HCG, Recombinant FSH, β-HCG, and Insulin.
- ADCC assay for biosimilars and different other assays like Ex Vivo assay, Cell-based assay, Receptor Binding Assay, Cytokine Release Assay, and ADA assay.
Veeda Group provides Integrated Discovery, Development & Regulatory Services with its multiple technology platforms:
- Exploratory toxicology studies
- Regulatory toxicology studies
- In vitro Bioassays
- Ex vivo Bioassays
The group also has the experience to handle a diverse range of Biotherapeutics like Therapeutic Monoclonal Antibodies, Insulin & Insulin Analogues, Cytokines, Low Molecular Weight Heparins, Biosimilars, Hormones & Biomarkers.
Veeda group has demonstrated capabilities to develop recombinant proteins such as non-glycosylated proteins and glycoproteins derived from either bacterial or mammalian host expression systems.
Bioassays in Preclinical Drug Development
Biological assays or bioassays are essential tools in preclinical drug development. Preclinical bioassays can be in vivo, ex vivo, and in vitro.
In vivo bioassays provide a more realistic and predictive measure of the functional effects of tests with reference drug products or standard material of defined potency, along with the application of statistical tools, study-specific lab techniques, and adherence to the well-designed study protocol.
These assays capture the complexity of target engagement, metabolism, and pharmacokinetics of novel drugs better than in vitro bioassays.
The most commonly used experimental mammals in in vivo efficacy assays are mice and rats. Occasionally other species may be used depending on the sensitivity & suitability of the assays.
Development and Validation of Bioassays
Bioassays are used as a screening method to identify the signals that indicate desired biological activity from a set of compounds. In general, two different types of signals can be generated by a bioassay, a linear dose-response and a sigmoidal (S-shaped) dose-response.
Since one solution does not fit all bioassays, it is good to evaluate and analyze the data to develop a precise approach to carry out each bioassay.
The life cycle stages of a bioassay are divided into:
Stage 1: Method design, development, and optimization
Stage 2: Procedure performance qualification
Stage 3: Procedure performance verification (fit for purpose)
Developing a bioassay that meets regulatory requirements and gets a drug product registered is a very complex process.
Developing a bioassay includes many strategies and tactical designs like selecting the correct in vivo platform, proper method or plate design, data analysis, system/ sample sustainability strategy, method implementation, method performance, and monitoring.
There are several steps to be followed for the development and validation of bioassays, such as dose-response and curve-fitting selection, development of reference, calculation of potency, bioassay characterization, design of bioassay calculator, standardization and automation of bioassay, and finally, evaluation.
Both method development and validation of bioassays include three fundamental areas:
- Pre-study (Identification and Design Phase) validation
- In-study (Development and Production Phase) validation
- Cross validation or method-transfer validation
During method development, assay conditions and procedures are selected that minimize the impact of potential sources of invalidity. Coming to the statistical validation for an in vivo assay, it involves four major components:
- Adequate study design and data analysis method
- Proper randomization of animals
- Appropriate statistical power and sample size
- Adequate reproducibility across assay runs.
Parallel group design, randomized block design, repeated measures design, and crossover design are the basic types of experimental designs used in in vivo assay.
The following are the key factors that should be kept in mind while designing an in vivo assay:
- All meaningful biological effects (pharmacologically) should be statistically significant.
- If biologically relevant assays are not present, then a range of plausible effects can be considered.
- The key endpoints should be well-defined before the beginning of the assay.
- Animals should be allocated randomly in an appropriate manner to the treatment groups.
- The dose levels should be selected appropriately. Dose and curve-fitting selection is among the most critical aspects of bioassay development. The dose is determined depending on the type of model used in the signal to fit the data. For Sigmoidal designs, a four- or five-parameter logistics (4PL or 5PL) model fits the data, whereas, for linear design, a parallel line analysis (PLA) model fits the data.
For a 4PL model, nine doses are recommended:
- Three doses in the lower asymptote
- Three doses in the upper asymptote
- Three doses in the linear range
In contrast, for a PLA model, a minimum of four doses is recommended. A minimum of three consecutive doses is required to plot the dose curve.
- The selection of control groups and time points to collect samples should be optimal.
- The design strategies should minimize variability and maximize information.
To understand the design, developments, and statistical validation of in vivo bioassay in more detail, reach out to us at https://www.veedacr.com. One can also read the guidelines mentioned by NIH by visiting the link:
https://www.ncbi.nlm.nih.gov/books/NBK92013/pdf/Bookshelf_NBK92013.pdf
References
- A. Little, “Essentials in Bioassay Development,” BioPharm International 32 (11) 2019
- Padmalayam, Ph.D., Assay development in drug discovery
- Zwierzyna M, Overington JP (2017) Classification and analysis of a large collection of in vivo bioassay descriptions. PLoS Comput Biol13(7): e1005641. https://doi.org/10.1371/journal.pcbi.1005641
- White JR, Abodeely M, Ahmed S, Debauve G, Johnson E, Meyer DM, Mozier NM, Naumer M, Pepe A, Qahwash I, Rocnik E, Smith JG, Stokes ES, Talbot JJ, Wong PY. Best practices in bioassay development to support registration of biopharmaceuticals. Biotechniques. 2019 Sep;67(3):126-137. doi: 10.2144/btn-2019-0031. Epub 2019 Aug 5. PMID: 31379198.
- F Chana and Hursh D, Bioassays through the Product lifecycle: Perspectives of CDER and CBER reviews.
- Haas J, Manro J, Shannon H, et al. In Vivo Assay Guidelines. 2012 May 1 [Updated 2012 Oct 1]. In: Markossian S, Grossman A, Brimacombe K, et al., editors. Assay Guidance Manual [Internet]. Bethesda (MD): Eli Lilly & Company and the National Center for Advancing Translational Sciences; 2004-. Bookshelf URL: https://www.ncbi.nlm.nih.gov/books/